A Link Between Viruses And Cancer
This is not the virus that sends you to bed for a couple of days with sneezing and the sniffles. This is not the virus that propels you to the closest bathroom to empty the contents of your stomach. This is not the virus that sends Ebola headlines screaming around the globe.
This is the virus that causes cancer: the oncovirus. And in its various forms, it causes at least 15 percent of cancers worldwide, according to the National Institutes of Health. Scientists who study cancer and viruses say that figure may be more than twice that much.
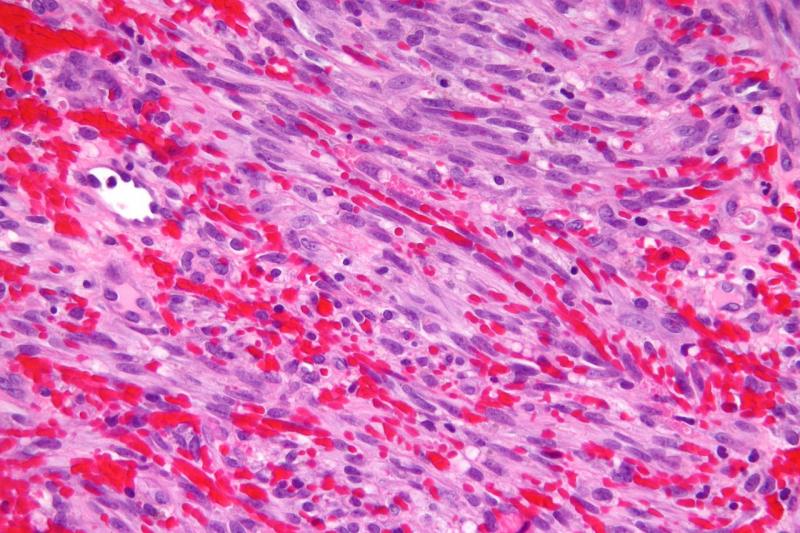
"We would like to understand the mechanism of how it causes cancer," says Shou-Jiang Gao, a USC molecular microbiologist who studies the herpes virus that causes Kaposi’s sarcoma, a type of skin cancer typically found in people with weakened immune systems, such as AIDS patients.
Gao points excitedly to a microscopic image on top of his lab's web page. It looks like a bunch of green tinsel from a Christmas tree, with glowing green orbs mixed in.
"See that?" he points. "That's cancer."
It is Kaposi’s sarcoma-associated herpesvirus (KSHV), which Gao studies.
"We know what pathway they target," Gao says.
Like a ninja slipping through a secret back door, the virus that causes Kaposi's sarcoma sneaks in through the body's complement system. Whenever a bacteria or virus enters the body, the immune system uses antibodies to find them. Sometimes, the antibodies are strong enough to prevent infection. But when they're not, the complement system kicks in, sending molecules found in the blood to attack. That causes inflammation to help fight off infections.
SEE ALSO: International Travel For Healthy Adults
But the virus that causes Kaposi's sarcoma sneaks around that by blending in. Unlike other viruses, it does not take over the cell's DNA and start giving orders, so the body does not know to send the immune response.
It's a little bit like the cartoon character Homer Simpson sitting cluelessly at the controls of the nuclear power plant while a nuclear meltdown unknowingly happens behind him. The body's immune system is like Homer Simpson. And the virus is the meltdown. Homer has no idea it is happening. Neither does the body.
Under the cover of that veil of unknowing, the virus hijacks the complement system. The molecules in the complement system just can't keep up. The virus replicates at super speed.
"They are much faster and much, much stronger. That's how they ultimately cause cancer," says fellow USC researcher Jae Jung.
This particular herpes virus does not change the cell's DNA until the very late stages of cancer, so the body thinks nothing is wrong.
Instead, the virus grabs part of the cell's genome, incorporates it into its own and uses the disguise to hide from the body's immune system.
"They change it a little bit to make it very strong," Jung says of the viruses and their use of the body's genes.
The genetic disguise gives the form of herpes time to replicate before the immune system can kick in. Because the virus is able to incorporate the body's genes into its own system, it's able to become more efficient than the body's immune system.
"So we carry the gun and they carry the gigantic bazooka," Jung says. "They catch our gun and make it like the bazooka they carry."
Jung says the body loses the arms race, which ultimately leads to the virus causing cancer.
The herpes virus that causes Kaposi's sarcoma isn't the only one that causes cancer. The human papillomavirus, or HPV, is a well-known example of a cancer-causing virus.
During last summer's annual Nobel laureate gathering in the lakeside town of Lindau, Germany, young scientists from around the world gathered around Zur Hausen like he was a rock star. He talked with them about his HPV studies, as well as what he's researching now.
Zur Hausen has moved on from HPV and has switched his focus to studying a potential link between viruses in beef and colon cancer. Zur Hausen has yet to produce any published results on his study, but calls the preliminary findings "promising."
He speculates that people may get colon cancer from eating virus-infected beef from dairy cows that are common in the U.S., Canada and Europe.
"For instance, yak meat in Mongolia, which is consumed at a larger rate or Zebu meat in India and also in Bolivia and a few other countries, Central Africa, don't seem to pose the same risk specifically as dairy cattle," zur Hausen says, pointing out that rates of colon cancer are much lower in Mongolia, India and other countries that consume different types of cattle than dairy cows.
He and his lab are trying to isolate the viruses in meat from dairy cows. If their study shows a link, there could be a potential to vaccinate cattle or people to prevent colon cancer, much like vaccinations are being used to prevent cervical cancer.
READ MORE: A Tranquil Setting For An Extreme Organism
The elderly Zur Hausen's take on the use of vaccinations is sometimes controversial. He's an advocate of vaccinating boys against HPV, which has hit resistance in the U.S. because HPV is associated with women and cervical cancer, not men, who don't have cervixes. But zur Hausen says even though males don't get cervical cancer, they are the ones who transmit HPV, which causes it, from woman to woman. HPV also causes anal, vaginal, penile and throat and neck cancers.
Zur Hansen’s view of the HPV vaccine resonates thousands of miles across the Atlantic, in the office of Martin Kast, the director of USC's medical biology program. Kast studies HPV and potential treatments for the virus and the cancers it causes.
Kast's office is adorned with pictures of he and his family with zur Hausen. He met the famous researcher a few years ago when USC awarded zur Hausen an honorary degree. And like zur Hausen, he believes the United States needs to do more to vaccinate against the virus that causes 70 percent of cervical cancers.
"The vaccine is marketed as a cervical cancer vaccine. Boys don't have a cervix, so how are we going to convince the parents of a boy that their boy needs to be vaccinated for cervical cancer?" Kast says, after pointing out that his son was among the first boys vaccinated against HPV. "It's a huge battle."
As of 2014, the U.S. Centers for Disease Control and Prevention reports only about 38 percent of girls in the U.S. have been vaccinated against HPV. The number of vaccinated boys is fewer than that.
Experts estimate about 80 percent of sexually active women will be infected by the virus by the time they are 50 years old. U.S. Centers for Disease Control and Prevention figures show more than 12,000 women in the U.S. are diagnosed with cervical cancer each year. More than one-third of them die. A vast majority of those cases are triggered by HPV.
So Kast is working on coming up with other ways than the vaccine to activate the immune response against the cancer-causing virus, which gets into the body's Langerhans cells. These are a type of immune-related cell on the skin and in the mucus layer of certain parts of the body.
Because HPV is in the Langerhans cells, the body doesn't realize it's infected, so it does not trigger the part of the immune system that deals with viruses. So the virus, much like a ninja, escapes the immune system under the cover of the Langerhans cells.
"Now that we have identified that mechanism, it means we think we have the Achilles heel of the virus," Kast says.
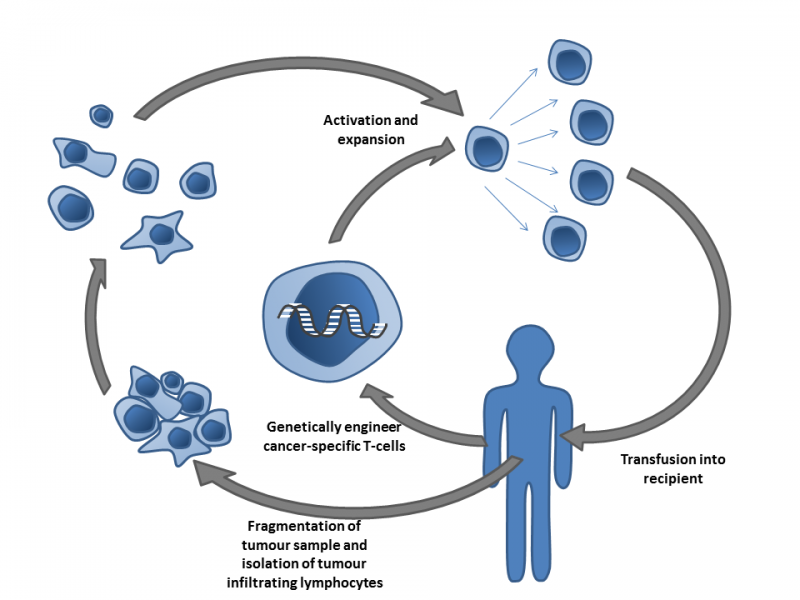
Researchers at USC have manipulated the infected Langerhans cells so the body's virus-attacking T-cells can detect the HPV in the cells. Kast calls this "reversing that immune escape." Basically, the body figures out how to shine a light on the sneaky ninja.
Drugs that help the body target and attack HPV could be put into a vaginal gel or on condoms to use before sexual intercourse, which is part of the project Kast is working on. Though he points out, that unlike the HPV vaccine, it would have to be used with each sexual interaction, much like how condoms are used to prevent pregnancy.
"It's certainly not as good as a vaccine would be, but if a vaccine is not taken up in the population, then finding an alternative is still very attractive," Kast says.
His lab plans to begin a clinical trial of such a drug at USC within the next year or so.
Another possibility to fight HPV may be a therapeutic vaccine, a type of vaccine used after an infection. The idea is to neutralize the virus so it cannot get into your cells, similar to taking away a ninja's weapons. The virus would still remain in your system, but it couldn't do any damage.
A therapeutic vaccine trains the body's own T-cells, which zero in on viruses, to detect tiny bits of the virus on the outside of HPV-infected cells. The T-cells then kill those cells to get rid of the virus. Getting rid of the cells gets rid of any developing cancer.
Work on attacking HPV and HPV-caused cancers from that angle is "going reasonably well," but Kast says it's not far enough along to put a therapeutic vaccine on the market.
Several similar T-cell treatments have gone all the way to the last clinical trial stage before Food and Drug Administration approval, but then failed in that last stage. Still, Kast says there is a lot of development of potential treatments in that area, even though such treatments could be very expensive.
But viruses with their ninja-like ways aren't always the enemy. In fact, as researchers have gotten to know the ninjas better, they've started to wonder if the viruses could be used for something positive.
Some researchers are studying how to use viruses to zero in on and kill cancer cells, a technique known as oncolytic therapy.
SEE ALSO: Preparedness For A Zombie Apocalypse
Former virologist Bill Phelps, who now works for the American Cancer Society, says it's not just a new drug, but an entirely new way to treat cancer, on top of radiation and conventional chemotherapy.
"After probably four or five decades of poking around and failing, including failing in patients, you're beginning to see some early hints of success with oncolytic therapy," Phelps says.
Oncolytic therapy researchers are still in very early stages, with what Phelps calls "very, small numbers" of patients studied. He says researchers have had some success in the past couple of years, but he doesn't necessarily credit advances in technology. More so, Phelps says failure has led to progress. As studies have failed to produce successful results, the scientists have been able to learn more about the cancer cells from those failures.
"You have to learn enough about how it works and maybe more importantly, why it doesn't work when you expect it to," Phelps says. "So I think by studying failures, more so than anything, is where you learn how to take the next step."
Immunotherapy, strengthening the body's immune system to fight off cancer on its own, seems to be slightly ahead of the development of oncolytic therapy, according to Phelps. With immunotherapy, patients' immune systems can be boosted with cell injections and by changes in diet. But Phelps says both immunotherapy and oncolytic therapy may be used together someday as complementary cancer treatment.
Oncolytic therapy does face an image problem, though.
"I think anytime you're adding a virus to a patient, you have to be concerned. And with cancer patients, there's a significant amount of immune suppression in many of them," Phelps says. "And so infecting immune-suppressed people is always a scary proposition."
But Phelps says if a cancer patient is faced with either oncolytic therapy with viruses or death, the decision is easy. Take the ninja. It's fast. It's efficient. It will kill only certain types of cancer cells.
"They're very powerful," Phelps says. "But you also have to be careful."
Reach Contributor Susan Valot here. Follow the Science Desk here.



